In addition to some more visible parts of the body, fat can infiltrate organs and gradually colonize their cells. This is what happens to the liver when we talk about steatosis or, more popularly, non-alcoholic fatty liver, the most widespread chronic pathology of this organ in the world: more than three in 10 people will suffer from it, according to a 2023 study published in the journal Hepatology.
Benjamín Polo Lorduy, head of the Digestive System service at the Fundación Jiménez Díaz University Hospital (Madrid), explains that the liver is “like a stone”, an organ in which it is difficult for any substance to infiltrate: “The fat, first of all, goes into the easiest areas: breasts, hips… When it enters the liver, it is very difficult to get it out”, he specifies. But why does that fat end up jumping out of those? easy areas to organs such as the liver? Beatriz González, specialist in the Endocrinology service at the Quirónsalud Sagrado Corazón Hospital (Seville), responds: “Adipose tissue can stretch up to a limit. That is, we have a maximum capacity to store fat at a subcutaneous level and, when this capacity is exceeded, it is deposited in other organs, such as the liver. That’s when we talk about liver disease associated with metabolic dysfunction.”
“When we notice an increase in abdominal circumference we should get back on track and go to the doctor. Almost 80% of people with fatty liver suffer from obesity”
Beatriz Gonzalez Aguilera Specialist of the Endocrinology Service of the Quirónsalud Sagrado Corazón Hospital (Seville)
The main challenge posed by fatty liver is its “invisible nature”, as explained by Rafael Esteban Mur, director of the Internal Medicine service at the Quirónsalud Hospital in Barcelona: “It does not produce symptoms or pain, especially in the early stages of the phenomenon. But there is a signal that should alert us: obesity.” Being overweight or obese, in fact, “is also correlated with a predisposition to other metabolic diseases such as diabetes or cardiovascular diseases”, adds González, who underlines: “When we notice an increase in the abdominal perimeter, we should get back on track and go to the doctor. Almost 80% of people with fatty liver suffer from obesity”.
Another clue that helps prevent this disease is the fatty liver index, an indicator that is calculated in some medical tests carried out at work and which, according to a study carried out by Quirónprevención – in whose medical tests this index is obtained – and recently published in the scientific journal of the Spanish Society of General Practitioners, allows for the early identification of people at risk of suffering from this pathology. It is also easy to estimate the body mass index (BMI), a measurement that Polo defines as “common but useful, which should alert us if it is equal to or greater than 25, even more so if we have pathologies such as high blood pressure, hypercholesterolemia or type 2 diabetes”.
Once we go to the doctor, there are several tools to detect an incipient fatty liver. The simplest test is a blood test, in which some serum markers are measured, such as transaminases, enzymes linked to metabolic processes which, “even if they have little sensitivity, if they are high they are a good indicator of hepatic steatosis”, specifies González. If there is a suspicion of liver disease, an abdominal ultrasound is performed to determine the level of fat infiltration in the organ: “From 20% we can talk about fatty liver”, specifies Polo.
“If the fatty liver persists and does not regress, cirrhosis occurs, a sort of ‘death’ of the inflamed and damaged tissue”

Rafael Esteban Mur Head of the Internal Medicine service at the Quirónsalud Hospital in Barcelona
Fibrosis is, in fact, the first malignant evolution of fatty liver. Dr. Mur summarizes the phases of this pathology as follows: “First we have fatty liver, steatosis. Then there is fibrosis, the appearance of scars in the organ and the beginning of cellular damage. If this condition is prolonged and does not regress, cirrhosis occurs, a type of death of that inflamed and damaged tissue, and the general dysfunction of the organ”.
This is how liver damage evolves
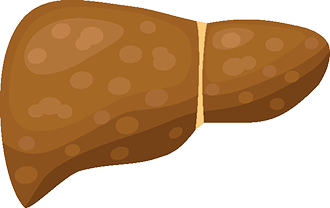
fatty liver
Fat infiltrates the liver and accumulates in the organ, causing it to enlarge.
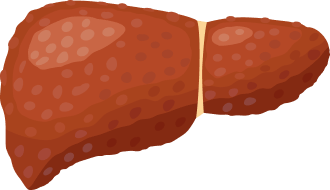
Fibrosis
As time passes, scarring begins to appear in the liver, the first signs of liver damage.
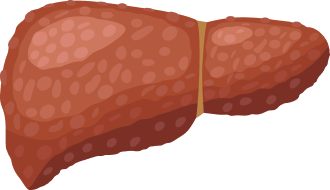
Cirrhosis
Scars caused by fibrosis harden. The affected liver tissue “dies” and stops functioning, causing dysfunction in the organ
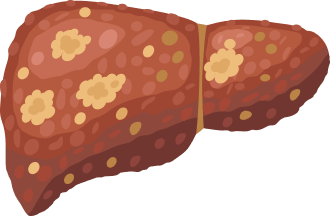
Cancer
If cirrhosis is left untreated, liver damage spreads and increases the risk of developing liver cancer, called hepatocellular carcinoma.
Source: Own elaboration based on the testimonies collected in the report.
Cirrhosis, the most advanced stage of liver damage, involves very disabling comorbidities, as Dr. Polo explains: “Varicose veins can appear in the esophagus, digestive bleeding, urinary retention problems… The degree of fibrosis must always be determined, which ranges from one (the mildest) to four (which indicates cirrhosis). The 20% of the most serious cases can result in hepatocellular carcinoma, which would be a liver tumor,” he continues.
When prevention and treatment meet
If in all pathologies prevention and treatment are somehow linked – to greater prevention, lesser and milder treatments -, in fatty liver this relationship takes on even more weight. Here what serves to anticipate the disease also serves to reverse it. There are two recommendations, explain the three specialists, to follow: «Adopt good eating habits based on the Mediterranean diet and do physical exercise, whether aerobic, two hours a week is fine, or anaerobic or strength training a couple of times a week», explains González.
“The problem is that we have very integrated low-calorie diets, with fast food, sugary drinks, rich in saturated acids and fructose. This increases the tendency to obesity”
Benjamin Polo Lorduy Head of the Digestive System Service of the Fundación Jiménez Díaz University Hospital (Madrid)
The recipe is simple and, in principle, convenient. And, as González estimates, it has immediate and notable effects on the patient’s condition: “Between 3% and 5% weight loss significantly reduces the amount of fat in the liver. And between 7% and 10% can reverse liver inflammation, although it is difficult to sustain this reduction with diet and exercise alone. In these cases, adds the doctor, “drug therapies can be useful in this weight loss.” And in more advanced cases, those with a BMI above 35 and comorbidities, “bariatric surgery (a reduction of the stomach) may be considered.”
Concern about this disease “is increasing”, explains Esteban Mur: “Fatty liver is already the main cause of liver cirrhosis in developed countries. It is a problem that we must address together with the industry and patients.” The complexity lies in the fact that the increase in fatty liver is linked to current consumption habits. We have very integrated low-calorie diets, with fast food, sugary drinks, rich in saturated acids and fructose… This increases the tendency to obesity. And awareness is also insufficient: we have less and less time to eat well and we are more sedentary, which worsens our conditions”, summarizes Polo.
To break this vicious circle, continues González, we must act on a small scale, improving what we have at hand: “Losing a little weight already changes the fatty liver a lot. This and always relying on expert hands. It is a reversible condition as long as we catch it in time.”



